Pharmacology for technicians 7th edition – Pharmacology for Technicians, 7th Edition embarks on an enlightening journey through the intricate world of pharmacology, equipping technicians with the knowledge and skills essential for safe and effective medication administration.
Delving into the complexities of drug administration, metabolism, and excretion, this comprehensive guide explores the mechanisms of drug interactions and their implications for patient care. Through real-world examples and practical insights, readers gain a deep understanding of the principles and practices of pharmacology.
Drug Administration
Drug administration refers to the process of introducing a drug into the body. Different routes of drug administration have advantages and disadvantages, and the choice of route depends on factors such as the drug’s physicochemical properties, the desired onset and duration of action, and the patient’s condition.
Oral Administration
- Advantages: Convenient, non-invasive, and cost-effective.
- Disadvantages: Can be affected by gastrointestinal absorption, first-pass metabolism, and patient compliance.
- Examples: Tablets, capsules, liquids
Intravenous Administration
- Advantages: Rapid onset of action, precise dosage control, and bypasses gastrointestinal absorption.
- Disadvantages: Invasive, requires skilled administration, and can cause adverse reactions.
- Examples: Injections, infusions
Intramuscular Administration
- Advantages: Faster onset of action than oral administration, bypasses gastrointestinal absorption.
- Disadvantages: Can be painful, may cause tissue damage, and requires trained personnel.
- Examples: Injections
Subcutaneous Administration
- Advantages: Slower onset of action than intramuscular administration, less painful, and easier to administer.
- Disadvantages: Can cause local irritation, and absorption may be variable.
- Examples: Injections
Transdermal Administration
- Advantages: Convenient, non-invasive, and provides sustained drug delivery.
- Disadvantages: Can be slow to take effect, and absorption may be affected by skin condition.
- Examples: Patches, gels
Factors Influencing Drug Administration Route
- Drug properties (e.g., solubility, stability)
- Desired onset and duration of action
- Patient’s condition and preferences
- Availability of skilled personnel
- Cost
Drug Metabolism and Excretion
Drug metabolism and excretion are essential processes that eliminate drugs from the body. Metabolism involves the chemical transformation of drugs into more water-soluble and excretable forms, while excretion involves the removal of drugs and their metabolites from the body.
Drug Metabolism
- Occurs primarily in the liver
- Enzymes involved: cytochrome P450 enzymes, glucuronosyltransferases
- Phases: Phase I (oxidation, reduction) and Phase II (conjugation)
Drug Excretion
- Primary route: Kidneys (urine)
- Other routes: Feces, sweat, saliva, breast milk
- Factors affecting excretion: Renal function, pH, drug binding
Factors Affecting Drug Metabolism and Excretion
- Age
- Liver and kidney function
- Genetic factors
- Drug interactions
Drug Interactions
Drug interactions occur when two or more drugs taken together produce an effect that is different from the effect of each drug taken alone. These interactions can be beneficial or harmful.
Types of Drug Interactions
- Pharmacokinetic interactions: Affect drug absorption, distribution, metabolism, or excretion.
- Pharmacodynamic interactions: Affect the drug’s mechanism of action or physiological response.
Consequences of Drug Interactions
- Increased or decreased drug efficacy
- Increased or decreased toxicity
- New or unexpected side effects
Common Drug Interactions
- Warfarin and aspirin: Increased risk of bleeding
- Digoxin and quinidine: Increased risk of digoxin toxicity
- CYP450 enzyme inhibitors (e.g., cimetidine) and antidepressants: Increased antidepressant levels
Mechanisms of Drug Interactions
- Altered drug absorption
- Competition for drug binding sites
- Induction or inhibition of drug-metabolizing enzymes
Drug Therapy for Specific Conditions
| Condition | Drug Class | Mechanism of Action | Examples |
|---|---|---|---|
| Hypertension | ACE inhibitors, ARBs, diuretics | Reduce blood pressure | Captopril, losartan, hydrochlorothiazide |
| Diabetes | Insulin, metformin, sulfonylureas | Lower blood glucose levels | Insulin glargine, metformin, glimepiride |
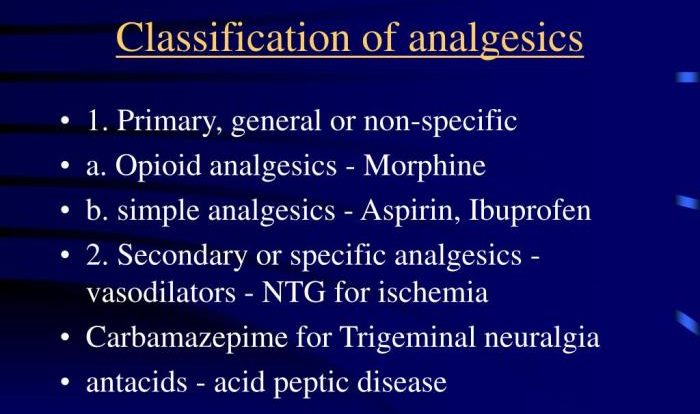
| Pain | NSAIDs, opioids, local anesthetics | Relieve pain | Ibuprofen, morphine, lidocaine |
Medication Errors: Pharmacology For Technicians 7th Edition

Medication errors are unintentional errors that occur during the medication use process. These errors can have serious consequences for patients.
Causes of Medication Errors
- Human factors (e.g., fatigue, distraction)
- Systemic factors (e.g., poor communication, lack of training)
- Drug factors (e.g., similar packaging, confusing names)
Consequences of Medication Errors
- Patient harm (e.g., adverse drug events, death)
- Increased healthcare costs
- Loss of patient trust
Strategies for Preventing Medication Errors, Pharmacology for technicians 7th edition
- Implementing electronic prescribing
- Standardizing medication names and packaging
- Improving communication between healthcare professionals
- Providing patient education
FAQ
What is the primary focus of Pharmacology for Technicians, 7th Edition?
Providing technicians with a comprehensive understanding of pharmacology, including drug administration, metabolism, interactions, and therapy.
How does the book address drug interactions?
Through a detailed exploration of the mechanisms and potential consequences of drug interactions, providing examples and strategies for managing them.
What practical aspects of pharmacology are covered?
The book includes real-world examples, case studies, and practical tips for safe and effective medication administration.